Evidence-informed Home Health Management
of Total Knee Arthroplasty
By: By Babatope Olusina, PT, DPT and Olaide Oluwole-Sangoseni, PhD, DPT, MSc.
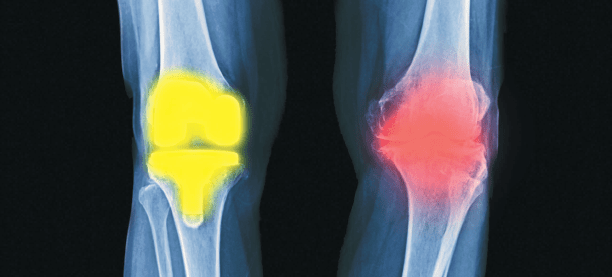
Osteoarthritis (OA) is a degenerative joint disorder that affects the articulating bones, the articular cartilage, and surrounding soft tissues. Other causes of joint pain and degeneration include rheumatoid arthritis (RA), osteonecrosis, post-traumatic degenerative joint disease, and other pathologic conditions. While joint pain is usually the first sign that prompts the decision to seek medical attention1, other symptoms soon develop, including but not limited to joint hypomobility and muscle weakness. The progression of the disease results in the development of functional limitations such as difficulties with transfers, gait abnormality, stair management, and completing activities of daily living (ADLs), eventually having negative impacts on work, pleasure, and quality of life.
The knee joint is the largest weight-bearing joint in the body, and chronic knee pain has been listed as a “leading cause of musculoskeletal disability in the United States (US)”. 2 Total knee arthroplasty (TKA) is the surgical replacement of the natural knee joint with a prosthesis. It was the first performed in the US in 1968, and with ongoing advances in the technique and materials used, significant progress has been made in its effectiveness and success rate. A 2010 prevalence study of TKA by Kremers el al3 estimated 1.52% in the entire US population, and 4.55% in those over the age of 50 years, have had TKA. Prevalence is higher in women as compared with men, and it increases with age. Inacio et al4 projects that the number of TKAs performed in the US will increase by the year 2050 to a prevalence of 2.58%, amounting to 2,854 procedures per 100,000 US citizens. Partial knee replacement is often performed when the degenerative changes are confined to a particular compartment of the knee and mostly in the younger patient. The PT management is similar to that of a TKA, as described later in this study.
Physical therapy (PT) plays a major role in the initial conservative management of the knee pain before TKA, not only for pain management but also to improve function and decrease the limitations afflicted by the condition. Following a TKA, the home health physical therapist is part of the multidisciplinary team approach that manages the patient upon discharge home. Our Home Health Agency (HHA) has developed protocols to manage these patient populations effectively. Based on previously established protocol with the referring Orthopedic Surgeon, a registered nurse (RN) completed the initial visit, performing a comprehensive assessment of the patient, including the past medical history (PMH), assessment and care of the surgical incision, medication review/training, and the OASIS elements. This HHA also has established protocol with other Orthopedic Surgeons where the PT is the admitting clinician. The initial PT evaluation consists of a detailed musculoskeletal assessment of the patient,
a review of the patient’s PMH, gait and balance evaluation, and a home safety evaluation. A PT plan of intervention is formulated to address noted impairments and functional limitations, with the patient’s self-stated goal as the endpoint.
The purpose of this case report is to highlight the physical therapy management of TKA in the home health setting.
Case Presentation:
The patient is a 50-year-old female office worker referred to home PT and Nursing following a right TKA revision due to instability and eventual failure of hardware. She resides with her husband in a single-level house, with 8 entrance steps, and she was fully independent with all of her functional mobility, including ambulating without an assistive device, but she was limited by right knee pain and the knee “locking up”.
Past Medical History:
Her PMH was significant for multiple comorbidities: Significant for Hypertension, Diabetes Mellitus, Hyperlipidemia, Asthma, Anemia, Cervical spine stenosis, Elevated Hemoglobin, Ehlers-Danlos syndrome, Depression, Metabolic syndrome, and Premature Ventricular Contraction (PVC). Her past surgical history is significant for Bilateral TKA, Anterior cervical discectomy with fusion, and Caesarean Section.
Medications:
- Acetaminophen, 500mg, 1 tab Q 4 hours as needed.
- Apixaban, PO, 2.5mg, 1 tab, twice daily
- Benadryl, 25mg, 1 cap daily
- Celebrex, 100mg, 1 cap twice daily
- Vitamin D3, 125mcg, 1 tab daily
- Crestor, 5mg, 1 tab daily
- Doxycycline Monohydrate, 40mg, 1 cap daily
- Ferrous Sulfate, 325mg, 1 tab twice daily
- Lisinopril-HCTZ, 20-12.5mg, 1 tab daily
- Metformin, 500mg, 1 tab twice daily
- Oxycodone, 5mg, 1 tab Q 4 hours, as needed
- Senna with Docusate Sodium, 8.6mg-50mg, 1 tab daily
- Singulair, 10mg, 1 cap twice daily
- Vitamin B12, 1,000mcg, 1 tab daily
- Cephalexin, 500mg, 1 tab 3x daily (started on 12/27/20)
Objective Examination and Assessment
Physical Status:
During her initial evaluation completed on 12/26/20, Valerie presented an alert and oriented to person, time, and place, and able to follow multi-level commands. She presented with hypomobility of her right knee (flexion ROM of 81 degrees and extension at negative 6 degrees) and weakness in her right quadriceps and hamstring muscle strength (2+/5 on the Manual Muscle Testing grade). She had difficulty with her bed mobility requiring close stand-by assistance, and she required supervision for her transfers. She was dependent on a pair of axillary crutches for ambulation using a 2-point gait pattern. She also used an antalgic gait pattern and exhibited poor arthrokinematics in the right knee. Her balance was assessed with the Timed Up and Go test (TUGT)5, with a score of 17 seconds; this identified her as having a high risk of falls.
Integumentary:
The patient’s right knee surgical incision was covered with “Aquacell”, a non-removable dressing on the day of PT evaluation. It was removed by skilled nursing during the subsequent visit on 12/29/20. PT assessed the patient’s surgical incision during all follow-up visits, for signs and symptoms of infection. This is part of agency protocol that all clinicians will assess surgical incision and document appropriately; coordination of care is performed weekly with the RN case manager.
Pain:
The patient’s pain level and description were assessed and documented during the initial PT evaluation and subsequent visits. The PT provided education to the patient and her husband regarding pain management strategies with her prescription analgesics, cryotherapy, and movement.
Clinical Impression:
Based on the hypomobility of her Right knee joint and the weakness of her right hamstring and quadriceps muscles, the International Classification for Functioning, Disability and Health (ICF) model ICD diagnosis of M25.661 (stiffness of right knee, not elsewhere classified), was made.
Plan of Care
PT determined that patient will benefit from skilled intervention with a frequency of 3 times per week for 3 weeks, per previously established protocol with referring surgeon. The intervention included therapeutic exercises (including a range of motion [ROM], strengthening exercises, and joint mobilization), functional mobility training (including bed mobility, transfer, gait, and stair training), instruction in-home exercise program, balance reeducation, safety education, equipment training, patient and caregiver education, and training, to progress her to independence in all areas.
- Patient has a diagnosis of Ehlers-Danlos Syndromes (EDS)6, a connective tissue disorder with joint hypermobility as one of its primary symptoms. Her therapeutic exercises, especially her ROM, were modified acccording to her symptoms and feedback. Therapeutic exercises prescription and progression was developed based on the phase of her rehabilitation, described as follows:
Days 1-10 acute phase (with emphasis on ROM, isometric and isotonic exercises)
- Right quadriceps isometric contraction in a supine positon, sustained for 5 seconds, 10 repetitions;
- Isometric exercises in supine and sitting position including hip flexion, knee flexion and extension (short and long arc quads), ankle doriflexion, and plantarflexion, 10 repetitions;
- Right knee flexion and extension active range of motion (AROM) and active-assisted range of motion (AAROM) in supine and sitting positions, 5 repetitions of in each direction, or fewer based on patient’s pain or feedback.
- Progression to the next phase (sub-acute) was based on decreased in overall pain and joint effusion and improvement in Right LE muscle strength.
Days 11-21 the sub-acute phase (with progression to advancing ROM, strengthening exercises, and joint mobilization)
- Right knee AROM/AAROM/passive range of motion (PROM) to facilitate full extension ROM and maximum flexion ROM, 5 repetitions in each direction.
- Grade I knee joint mobilization in sitting and supine positons, to improve flexion and extension ROM, with close monitoring of her pain and to prevent hypermobility in either direction, 1-2 repetitions.
- Strengthening exercises using gravity and body weight for resistence, including hip flexion, extension, and abduction; knee flexion and extension (shot and long term arc quads); standing ankle dorsiflexion and plantarflexion, 2 x 10 repetitions.
- Use of eccentric muscle action to facilitate improvement of VMO strength, due to patient’s mild extension lag during SAQ and LAQ, 10 repetitions.
Home exercise program (HEP) – the patient was instructed to perform her HEP 2-3 times daily. HEP was upgraded from Phase 1 to Phase 2 as the joint effusion and pain decreased, the right LE muscle strength and coordination improved.
- Functional mobility training – The therapist provided verbal and visual instructions to the patient to quickly teach bed mobility and transfer techniques to progress her independence in both areas. Gait training with a pair of axillary crutches, emphasizing the proper use of the 2-point gait pattern and ensuring the crutches support the right LE, was performed. PT emphasized the need to increase right knee flexion ROM during the non-weight bearing phase of gait and facilitate full knee extension at heel strike. She was started on gait training with a one-handed device by the end of the second full week and progressed to independence by the end of her 3 weeks of home PT.
- Balance reeducation – transitional weight-shifting patterns in the anteroposterior and lateral directions in standing, facilitating increased weight bearing on the surgical leg. Later progressed to using a narrow base of support (BOS) in a modified tandem position, where she initially required contact guard assistance and later progressed to supervision level.
- Patient education: PT provided detailed instruction to the patient and her husband regarding pain and joint effusion management, signs and symptoms of DVT and infection at the wound site, and edema management. Patient education was specific to the home exercise program. Several studies have identified pain, fear of DVT, and edema as the most common reasons patients visit to the emergency room. (5-7) Therefore, our agency emphasizes patient education regarding symptoms management and patients’ expectations of their recovery roadmap. Safety education was provided, emphasizing the patient safely navigating her house with 2 cats and 2 small dogs underfoot. Her husband was instructed to, and he ensured a clear path to the bathroom from her bed, and he provided assistance that patient required for her first few shower transfers. During her fourth HHPT visit on 1/4/21, the patient reported feeling sick, dizzy, and nauseous after completing her supine and sitting exercises. Her vital signs were initially checked at the time of the therapist’s arrival, and they were within normal for the patient. She was assisted back to the couch, and her vital signs were re-checked; her blood pressure was now 91/53 mmHg, pulse was 94 beats per minute, and respiratory rate was 20 per minute, and her oxygen saturation was 98%. Further, the patient was diaphoretic and quite anxious. The PT re-assured the patient and provided moving air to cool her down. After about 5 minutes in a supine position with her lower extremities elevated, she reported feeling “somewhat better”. Her vital signs were re-checked – BP was 91/59 mmHg; pulse at 93 beats per minute; respiration at 16 per minute, and oxygen saturation at 98%. The patient’s surgeon’s office was contacted and informed about the incident. Her primary care physician (PCP) was also informed per the patient’s request. Both physicians agreed with the therapist that the patient did not require emergency care because her oxygen saturation remained within normal range, and she recovered in terms of her subjective feeling. PT ruled out possible Pulmonary Embolism (PE) using Well’s Criteria and ruled out possible DVT. She subsequently missed the next scheduled session on 1/6/21; even though she reports feeling better, she asked for another day to rest before resuming PT. She had a follow-up appointment with her primary care physician on 1/11/21 and was started on an iron supplement for postoperative anemia.
Outcomes
The patient completed 8 of 9 planned HHPT visits, and she had progressed to independent bed mobility and transfers by her third visit on 12/30/21. By the end of the 3rd week her progress was as follows:
- ambulating independently without an assistance device for 180 feet inside her house and with one crutch on uneven surfaces
- modified independent level managing her 8 entrance steps
- right knee AROM at 0-122 degrees.
- right quadriceps and hamstrings muscle strength at 3+/5 MMT scale.
- balance score of 12 seconds TUGT
- most postoperative anemia symptoms were resolved
- independent level with all of her ADLs
Discussion
The patient’s plan of care was developed based on a combination of her impairments following her right TKA, functional limitations, and goals. She made steady progress towards her stated goals of independence with all of her functional mobility and all of her ADLs, without pain and locking up of her Right knee joint. The patient regained full AROM of her right knee joint and regained muscle strength to engage in her regular activities. She progressed to and demonstrated independence with all of her mobility and planned to resume telecommuting the following week once cleared by her surgeon.
During HH services, the patient was diagnosed with postoperative anemia by her PCP, which is common among surgical patients.7 Following the initial incidence, her vital signs and symptoms were monitored more frequently. Her surgeon and PCP were contacted to report her symptoms, and because the patient was discharged from home health skilled nursing services on 12/29/21, the PT provided education to the patient regarding the possible drug interaction of her iron supplement prescribed by her PCP. Ferrous Sulfate can bind to Doxycycline in the Gastrointestinal tract, which may decrease their absorption and bio-availability. They should be taken 3-4 hours apart to avoid or minimize this interaction. The therapist also provided education to the patient and her husband regarding food rich in Iron to complement her medication.
Several studies have identified the common reasons for visits to the emergency room after TKA. (7-9) A study reported 15.6% of ED visits were for swelling, and 15.8% were uncontrolled pain.8 Another study reported that among patients who had ED visits after THA and TKA, the primary diagnosis in 17.84% was pain.9 To decrease unnecessary visits to the ER, our agency has developed a comprehensive education program for post-op THA and TKA patients. PTs share the information with the patient on the first visit regarding the red flags of infection and possible DVTs; and education regarding pain and edema management. The same information is reviewed on the 2nd and 3rd visits until the patient can verbalize the previously provided information.
This case report highlights the effective management of a TKA patient in the HH setting while incorporating the patient’s unique PMH and postoperative complications. Her exercise program and joint mobilization were modified to accommodate her Ehlers-Danlos condition and her vital signs more closely monitored with the postoperative anemia. Her exercise program was progressed from the initial set more suited for the immediate acute phase to more advanced exercises in the sub-acute phase. She was progressed to independent ambulation without an assistive device on a level surface and with a one-handed device on uneven surfaces.
About the Authors
Babatope Olusina, PT, DPT, Certificate of Advanced Competency in Home Health (APTA Home Health Section). He is a member of the APTA and Home Health section. Dr. Olusina now works for a home health agency in Richmond, VA, but previously owned and ran a Contract Therapy Staffing Company.

Dr. Olaide Oluwole-Sangoseni, PhD, DPT, MSc, GCS, is an associate professor of physical at Maryville University of St. Louis. She is a Board Certified Geriatric Specialist and a home health PT. Dr. Sangoseni is an advanced physical therapy clinical specialist degree in neuro-orthopedics from the University College London, England. She is an APTA credentialed clinical instructor. She can be reached at [email protected].
References
- Zhang Y, Jordan JM. Epidemiology of Osteoarthritis: Clin Geriatric Med.2010 Aug: 26(3): 355-369
- Jette DU, Hunter SJ, Burkett L, et al. Physical Therapist Management of Total Knee Arthroplasty: Physical Therapy. 2020 Aug; 100(9): 1603-1631
- Kremers HM, Larson DR, Crowson CS, et al. Prevalence of Total Hip and Knee Replacement in the United States. J Bone Joint Surg Am. 2015 Sep 2; 97(17): 1386-1397
- Inacio MCS, Paxton EW, Graves SE et al. Projected increase in total knee arthroplasty in the United States- an alternative projection model. Osteoarthritis Cartilage. 2017; 25: 1797-1803
- Centers for Disease Control and Prevention: National Center for Injury Prevention and Control. STEADI Tools. https://www/cdc.gov/steadi/pdf/TUG Test-print.pdf. Published 2017.
- Corrado B, Ciardi G. Hypermobile Elhers-Danlos syndrome and rehabilitation: taking stock of evidence-based medicine:a systematic review of the literature. J Physical Therapy Science. 2018 Jun; 30(6): 843-847.
- Perelman I, Winter R, Sikora L, et al. The Efficacy of Postoperative Iron Therapy in Improving Clinical and Patient-Centered Outcomes Following Surgery: A Systematic Review and Meta-Analysis. Transfusion Medicine Reviews, 2018 April, 32:2, 89-101.
- Kelly MP, Prentice HA, Wang W, Fasig BH, Sheth DS, Paxton EW. Reasons for ninety-day emergency visits and readmissions after elective total joint arthroplasty: results from a US integrated healthcare system. J Arthroplasty. 2018;33(7):2075-2081. doi:10.1016/j.arth.2018.02.010
- Finnegan MA, Shaffer R, Remington A, et al. Emergency Department Visits Following Elective Total Hip and Knee Replacement Surgery: Identifying Gaps in Continuity of Care. Journal of Bone and Joint Surgery: 2017 June 21. 99 (12), 1005-1012.