Evidence-informed Home Health Management
of Total Hip Arthroplasty
By: By Babatope Olusina, PT, DPT and Olaide Oluwole-Sangoseni, PhD, DPT, MSc.
Osteoarthritis is a degenerative joint disorder that affects the articular cartilage, underlying bone, and surrounding soft tissues. It is the most common form of joint disease in the United States (US), with an estimated prevalence of 27 million people,1 with an occurrence of about 10% in men and 13% in women, over the age of 60 years. 2 Hip osteoarthritis accounts for about 70% of total hip arthroplasties (THA) that are performed in the US due to severe pain, which limits the individual’s functional mobility and negatively affects his/her activities of daily living (ADLs), eventually limiting his/her participation in work and leisure activities. 3 Other indications for THA include but are not limited to trauma and osteonecrosis of the femoral head.4
THA is the surgical replacement of the natural hip joint with a prosthesis. 3 The first THA procedure was completed in the US in 1969 and as the procedure has grown in incidence, the technique has evolved and its efficacy has improved. 2,4 A 2010 prevalence study estimated 2.34% of individuals over the age of SO years in the United States have had THA, corresponding to 2.5 million people (1.4 million women). 4 A detailed breakdown of their study revealed a prevalence of 0.58% at age SO years, increasing to 1.49% at sixty years, 3.25% at seventy years, 5.26% at eighty years, and 5.87% at ninety years of age.4 The original or more popular technique is the posterior or posterolateral approach, with its associated precautions (no hip flexion above 90 degrees, no adduction beyond the midline, and no internal rotation of the surgical hip joint).
In the 1980s, an anterior approach was developed and gained popularity because of improved early outcomes in terms of pain and early functional recovery. 5 Hip hemiarthroplasty is the surgical removal of one of the components of the hip joint, most often the femoral head. Although it is less invasive, the Physical Therapy assessment and management will follow a similar path as for a THA.
Home health physical therapists (HHPT) are part of the multidisciplinary team-approach called upon to manage these patients upon their return home. Orthopedic surgeons seek the involvement of physical therapists (PT), as movement specialists, to facilitate the recovery and rehabilitation of THA patients to maximize their return to full function and participation in the activity. In consultation with the orthopedic surgeons, our home health agency established protocols that can be customized to fit the individual patient’s desired outcomes and surgeon’s preferences. These protocols guide the first few weeks of in-home rehabilitation before the transition to outpatient physical therapy. As a HHPT with a weekly caseload of about 50 percent of total hip and total knee arthroplasty patients, I recognize that no two patients’ status post-THA is the same.
The Medicare home health Conditions of Participation (CoP) require that a comprehensive assessment of each patient be performed by the admitting clinician to start the episode of care. This assessment includes the patient’s past medical history (PMH); a complete review of the patient’s medications, including any changes in dosage and patient’s response; and the integumentary assessment, all of which go into the process of formulating the patient’s plan of care.
Because most home health patients have multiple diagnoses, the evaluating PT incorporates the patient’s past medical/surgical history and the patient’s prior level of function into his/her physical therapy plan of interventions. A detailed assessment of the patient’s home is an essential aspect of the initial visit, as safety hazard/fall risks can be identified, and safety education and recommendations can be immediately communicated to the patient and their caregivers. The purpose of this case report is to highlight the physical therapy management of a THA in the home health setting with a focus on adapting exercise program based on pain and muscle fitness indices.
Case Presentation:
The patient is an 81-year-old female, retired nurse admitted to HHPT following right THA revision with weight-bearing as tolerated precautions. She resides alone in a single level house in a 55+ Age-in-Place community. Before this surgery, she was fully independent with all of her functional mobility, occasionally using a standard straight cane for ambulation. She was independent with all activities of daily living (ADL)s and was active in her community, participating in group exercise sessions every week.
Past Medical History:
Her PMH was significant for multiple comorbidities: hypertension, atrial fibrillation, type 2 diabetes mellitus, anxiety, neuropathy, general osteoarthritis, vertigo, history of lumbar laminectomy and fusion in 2017, reflux disorder, cystocele with prolapse, and recent urinary tract infection. Initial THA was performed in 2002; she had a dislocation in 2017, which resulted in persistent hip joint pain afterward.
Current Medications included:
• Apixaban, PO, 2.5mg, 1 tab, twice daily
• Diltiazem, PO, 240mg, 1 tab daily
• Norvasc, PO, 5mg, 1 tab PRN, if diastolic is above 90mmHg
• Pepcid, PO, 10mg, 1 tab Q 8 hours
• Xanax, PO, 0.5mg, 1 tab daily
• Tramadol, PO, 50mg, 1 tab Q 6 hours
• Purelax PO, 17gram/dose, 1 tab twice daily
• Potassium Chloride, PO, 20mEq, 1 tab twice daily.
• Tylenol Extra strength, PO, 500mg, 2 tabs Q 8 hours
The patient stated her goal is to return to walking independently without the walker.
Objective Examination and Assessment
Physical Status:
On examination, “Nanette”(a pseudonym) was alert and oriented to person, place, and time, and able to follow a multi-level command. She presented with hypomobility of the hip joint and weakness of the proximal muscles of the surgical lower extremity. She required contact guard/minimal assistance to assist her right lower extremity into the bed during bed mobility assessment. She required close stand-by-assistance of the therapist for sit to/from stand and bed to/from chair transfers due to She was dependent on a rolling walker for ambulation, with forward-flexed trunk posture over the device, using a 2-point antalgic gait pattern. The Timed Up and Go test (TUG) was performed, with the “Nanette” requiring 36 seconds to complete. 6 A time greater than 20 seconds is indicative that the patient is dependent on transfers and confirms homebound status. 6 The family had hired a private duty company to provide personal care assistance for several hours during the day to assist her in the first 3 weeks.
Integumentary:
Because the initial home PT evaluation was on the same day as the nursing start of care (SOC) visit, PT evaluation referred to the nursing integumentary assessment. However, the physical therapist assessed the surgical incision on each subsequent visit, per our agency protocol, performing dressing changes when needed. The status of the wound was documented and presented at the interdisciplinary case conference with the registered nurse as required.
Pain:
Per Medicare CoP, Nanette’s pain was evaluated on the initial examination and all subsequent visits, using a numeric pain rating scale (0-10) and verbal description. She rated her pain at level 5/10; her goal was to be pain-free by discharge. The expectation was a gradual decrease in the pain level, and any movement in the other direction and/or a new type of pain warrants additional evaluation.
Clinical Impression:
Based on the hypomobility of the hip joint and weakness of the proximal muscles of the hip and pelvis, the International Classification of Functioning, Disability and Health (ICF) model diagnosis of M25.651 or 652 (stiffness of hip joint, not elsewhere classified) was made.
Plan of Care
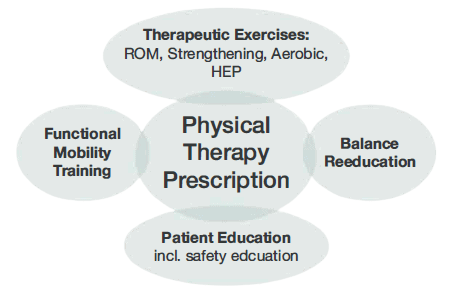
It was determined that Nanette would benefit from a skilled PT intervention frequency of 2 times per week for 4 weeks. Her exercise prescription consisted of joint mobilization, ROM and strengthening exercises, instruction in a home exercise program (HEP), functional mobility training (including bed mobility, transfer, and gait training), balance reeducation, equipment training, safety education, to progress to independence in all areas (Figure 1).
Since the pain was the chief complaint, it was used as one of the outcome measures. Pain medication was to be taken an hour before the PT session. The patient’s pain level was expected to decrease to level 1/10 at discharge.
- Therapeutic exercises on the day of the examination consisted of:
- Isometric contraction of the quadriceps and bilateral gluteal muscles sustained for 5 seconds or until fatigue.
- Isotonic exercises, including hip abduction (in standing), hip/knee flexion (in supine via heel slide) and knee extension (in sitting), ankle dorsiflexion and plantarflexion (in supine), up to 15 repetitions or until fatigue, using BORG rate of perceived exertion (RPE) score with a target score of 14 on the 6-208 scale.8 The PT’s focus was on increasing muscle endurance using a high repetition approach. The patient’s positioning during exercise was modified in sitting and standing due to a history of chronic acid reflux; she was unable to tolerate supine lying.
- Exercise progression/upgrade included gradual addition of hip flexion, abduction, and extension in standing for muscle strengthening-an upgrade of knee flexion, ankle dorsiflexion, and plantarflexion in standing using gravity and bodyweight resistance. Exercise intensity was based on RPE, and the type of exercise was the final two weeks to include external hip rotation in the supine position.
- Home Exercise Program (HEP): The patient was instructed to perform the aforementioned exercises as her HEP 2-3 times daily on the days that the PT is not scheduled, to maximize her progress and to progress her towards her stated goal. Nanette’s adherence was crucial to her overall recovery, stated personal goal, and physical therapy outcome. HEP adherence was monitored through direct open-ended questions and requested demonstrations during subsequent visits. Nanette was provided education to encourage cooperation with the overall plan of care.
- Functional mobility training included bed mobility training with safety instructions given to ensure the patient adhered to the THR precaution during supine to sit and sit to supine mobility. Transfer training included regular sit to/from stand, toilet transfers, shower and tub transfer training, and, later, car transfer training in preparation for discharge. The patient received gait training with the rolling walker, with verbal and visual instructions provided to address the deficits and impairments noticed during her initial examination. This patient received instructions for postural reeducation, and to increase stance time and the amount of weight-bearing in her right LE. As her pain subsided 2-3 points, and her right LE muscle strength improved, she was progressed to the use of a standard cane first on level surface, and later on uneven surfaces. Just before discharge, the patient was progressed to gait training without an assistive device.
- Balance reeducation in standing started with transitional weight-shifting patterns in the sagittal and coronal planes. The verbal emphasis was on maintaining upright trunk posture, increasing stance time on the surgical leg, and improving the amount of weight-bearing. The first progression of this was to perform the same activities without upper extremity support. The next progression was the use of transitional stepping patterns in the sagittal and coronal planes. These activities were performed to improve the muscle stabilization action around the replaced hip joint, as well as improve the patient’s confidence in the ability of the surgical hip to sustain her weight. This is essential in the progression of gait training from a walker to a cane, and eventually to ambulating without a device.
- Patient Education Patient education was a multi-pronged approach. The patient demonstrated a high level of health literacy; therefore, patient education was a multi-pronged approach. The PT provided education about Nanette’s THA precautions, with emphasis on observing these precautions as she goes through her day-to-day activities. Nanette’s precautions included avoiding turning towards the affected side, sitting in a low chair, and during supine to/from sitting, as these are some of the times when a patient is most likely to break the precautions. Safety education was provided in direct correlation to the safety hazards identified during the initial examination visit and other sessions. Nanette had area rugs in her walking path and a narrow path to her side of the bed. The PT provided suggestions and education regarding fall risks and prevention. Her bed was rearranged to allow a wider path to fit the walker. Area rugs were removed throughout the home. Also, caregivers (daughter and paid caregiver) were provided with education on a variety of topics, including Nanette’s home exercise program, signs, and symptoms of a deep venous thrombosis (DVT), pain medication management, the application of cold modalities for pain management, and if and when to seek medical attention. Researchers have suggested that there is an emergency room visit rate of about 13.4% in the first 90 days following THA, and the most frequent reasons are swelling (15.6%) and uncontrolled pain (12.8%).7 A study by Saleh et al documented these same common surgery-related reasons accounted for emergency room (ER) visits in about 35% of patients.9 These studies underscore the role of home health professionals in patient education regarding the careful assessment and management of swelling and pain in this population, as well as identifying patients that need to be referred to the ER for further evaluation immediately. This PT utilizes Wells’ Criteria for DVT10 as a clinical tool whenever there is concern about a possible DVT.
Outcomes
The patient achieved independence with her bed mobility by the first session of week 2 (3rd visit), and independence with her sit to/from stand and chair to/from bed transfers by the end of the second week (4th visit). She demonstrated independence with her shower stall and tub transfers by the third week (6th visit) and independence with car transfer in the 4th week. The patient progressed to gait training with a standard cane by the 3rd week. She had progressed to independence with gait training on level and uneven surfaces, including on her inclined driveway and to her community mailbox, which is about 450 feet away from her front door, with a numeric pain score of 0/10. Her functional score improved from 36 seconds at initial evaluation to 12 seconds using the TUG test. This score correlates with independence in all transfers and activities of daily living. Her right hip muscle strength had improved to 3+/5, and the patient demonstrated independence with her HEP. Nanette had achieved pain-free status by the final visit.
Discussion
This patient presented with several impairments that created limitations at the body function level as well as at the activity and participation level, 11,12 as laid out above with the ICF model.
The HHPT used his/her expertise to provide an individualized, person-centered, evidence-informed treatment in the management of this patient. The plan of care was based on the interdisciplinary protocol developed by the surgeon and the home health agency, to help achieve the goals she stated as important to her. Nanette was motivated to return to driving and get back to her normal social life with her friends in the 55+ Age-in-Place community where she resides. The patient had multiple episodes of elevated blood pressure that warranted the notification of her primary care physician (PCP). To err on the side of caution, our home health agency policy requires physician notification for any systolic above 150 and diastolic above 90mmHg. Although her PCP decided not to take any immediate action, her blood pressure was carefully assessed at the start of each visit and response monitored throughout the interaction. The patient had a medical history of anxiety, which sometimes played a role in her exercise response and feedback to the therapist, especially related to her RPE rating and response. She required frequent reassurance, and it was well managed afterward.
Further, consistent with her medical history, constant adjustments had to be made based on observations and findings at the beginning of each visit. Some of her exercises were modified, considering her history of back pain and surgery to avoid aggravating old symptoms. She received a reiteration of education regarding home safety and community re-entry in the last week of the HHPT visit.
Nanette was discharged from home health nursing services in her second week and was discharged to outpatient therapy upon completion of her 8th and final visit. She planned to start driving, first inside her community, once she was released from home health services. An anonymous satisfaction survey was mailed to her by the agency after discharge, and she expressed her satisfaction to the therapist on her last visit, showing how quickly she was progressed to independence with physical therapy. This case report demonstrates a successful progression of an individual with a posterior approach THA from acute care to return to community living through a three-week course of HH services.
About the Authors
Babatope Olusina, PT, DPT, Certificate of Advanced Competency in Home Health (APTA Home Health Section). He is a member of the APTA and Home Health section. Dr. Olusina now works for a home health agency in Richmond, VA, but previously owned and ran a Contract Therapy Staffing Company.

Dr. Olaide Oluwole-Sangoseni, PhD, DPT, MSc, GCS, is an associate professor of physical at Maryville University of St. Louis. She is a Board Certified Geriatric Specialist and a home health PT. Dr. Sangoseni is an advanced physical therapy clinical specialist degree in neuro-orthopedics from the University College London, England. She is an APTA credentialed clinical instructor. She can be reached at [email protected].
References
- Lespasio MJ, Sultan AA, Piuzzi NS, et al. Hip osteoarthritis: a primer. Perm J. 2018;22:17-084. DOI: https://doi.org/10.7812/TPP/17-084
- United States Bone and Joint Initiative: The Burden of Musculoskeletal Diseases in the United States (BMUS), Fourth Edition, 2020. Rosemont, IL. Available at http://www.boneandjointburden.org. Accessed on June 15, 2020
- Siopack JS, Jergesen HE. Total hip arthroplasty. West J Med. 1995;162:243-249, 1995
- Kremers HM, Larson DR, Crowson CS, et al. Prevalence of total hip and knee replacements in the United States. J Bone and Joint Surgery. 2015: 97(17): 1386-1397
- Wang Z, Hou JZ, Wu CH, et al. A systematic review and meta-analysis of direct anterior approach versus posterior approach in total hip arthroplasty. J Orthop Surg Res. 2018;13(1):229. Published 2018 Sep 6. doi:10.1186/s13018-
018- 0929 - Centers for Disease Control and Prevention: National Center for Injury Prevention and Control. STEADI Tools. https://www.cdc.gov/steadi/pdf/
TUG_Test-print.pdf. Published 2017. Accessed on June 20, 2020 - Kelly MP, Prentice HA, Wang W, Fasig BH, Sheth DS, Paxton EW. Reasons for ninety-day emergency visits and readmissions after elective total
joint arthroplasty: results from a US integrated healthcare system. J Arthroplasty. 2018;33(7):2075-2081. doi:10.1016/j.arth.2018.02.01 O - Williams N. The Borg Rating of Perceived Exertion (RPE) scale. Occupational Mede.2017; 67(5):404-405, https://doi.org/10.1093/occmed/kqx063
- Saleh A, Faour M, Sultan AA, Brigati DP, Molloy RM, Mont MA. Emergency department visits within thirty days of discharge after primary total hip arthroplasty: a hidden quality measure. J Arthroplasty. 2019;34(1):20-26. doi: 10.1016/j.arth.2018.08.032
- Wells PS, Anderson DR, Rodger M, et al. Evaluation of D-dimer in the diagnosis of suspected deep-vein thrombosis. N Engl J Med. 2003 Sep
25;349(13):1227-35. - Klapwijk LC, Mathijssen NM, Van Egmond JC, Verbeek BM, Vehmeijer SB. The first 6 weeks of recovery after primary total hip arthroplasty with fast track [published correction appears in Acta Orthop. 2018 Feb;89(1):140]. Acta Orthop. 2017;88(2):140-144. doi:10.1080/17453674.2016.1274865
- Bahardoust M, Hajializade M, Amiri R, Mousazadeh F, Pisoudeh K. Evaluation of health-related quality of life after total hip arthroplasty: a case-control study in the Iranian population. BMC Musculoskelet Disord. 2019;20<1>:46. Published 2019 Jan 31. doi:10.1186/s12891-019-2428-0